Lung Cancer Screening Program: Early Detection Saves Lives
On May 2, 2023, the Australian Government announced a significant investment of $263.8 million over four years to establish the national Lung Cancer Screening Program (LCSP). This program aims to improve early detection of lung cancer, the leading cause of cancer death in Australia.
What is the Lung Cancer Screening Program?
Lung cancer screening is a new program being rolled out in Australia in July 2025. It aims to:
- Reduce lung cancer deaths and complications.
- Support smoking cessation throughout the screening process.
The effective integration of smoking cessation is essential to LCSP. The maximum reduction in mortality is achieved with a combination of smoking abstinence and LDCT screening.
Who is the LCSP for?
The program offers screening to high-risk individuals:
- Aged 50-70 years old
- Current or former smokers meeting specific criteria
Participants can be referred by a healthcare professional or via a primary care provider of their choice. Mobile LDCT scan options will be available in areas with limited radiology services.
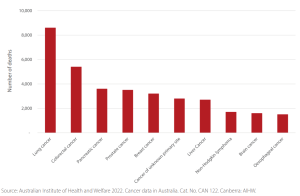
Key Statistics: Lung Cancer
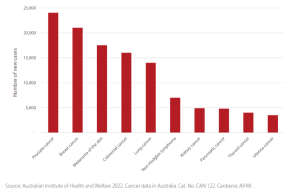
- High Mortality Rate: In Australia, lung cancer is the most common cause of cancer death, with over 8,000 deaths annually.
- Rising Cases: The number of new lung cancer cases diagnosed is on the rise in Australia, with over 14,272 diagnosed in 2023.
- Disparity Among Indigenous Australians: Indigenous Australians are disproportionately affected by lung cancer, being twice as likely to be diagnosed and die from the disease compared to non-Indigenous Australians.
- Importance of Early Detection: Survival rates for lung cancer are significantly higher when detected early. The five-year relative survival rate for stage I lung cancer is 67.7%, compared to just 3.8% for stage IV.
Importance of Early Detection
Early detection is crucial for improving lung cancer survival rates. Currently, most diagnoses occur at advanced stages when treatment options are limited. The five-year survival rate for stage I lung cancer is a staggering 67.7%, compared to just 3.8% for stage IV. Early detection through low-dose CT (LDCT) scans can significantly reduce lung cancer deaths.
Two large clinical trials (NELSON and ILST) have provided evidence that early detection via low-dose CT (LDCT) imaging in high-risk populations reduces the number of deaths from lung cancer, highlighting the need for developing such a program to improve lung cancer outcomes in Australia.
Indigenous Australians and Lung Cancer
Indigenous Australians are disproportionately affected by lung cancer. They are twice as likely to be diagnosed and die from the disease compared to non-Indigenous Australians. Cancer Australia reports lung cancer is the highest cause of cancer mortality in this population, nearly five times higher than colorectal cancer, the second leading cause.
Development of the National Lung Cancer Screening Program
Following the 2020 Lung Cancer Screening Enquiry (LCSE) report by Cancer Australia, a collaborative effort between Cancer Australia and the Department of Health and Aged Care began in July 2021 to design and assess the feasibility of a national LCSP.
This process involved extensive stakeholder engagement, particularly with Aboriginal and Torres Strait Islander representatives, to ensure the program addresses the unique needs of Indigenous Australians.
The representatives included Aboriginal health workers and practitioners, Indigenous smoking coordinators, Aboriginal liaison officers and cancer care coordinators, researchers, policymakers, and consumers.
Cancer Australia also received independent advice from MSAC. This included the creation of a new Medicare Benefits Schedule for LDCT scans, to support the early detection of lung cancer in asymptomatic high-risk individuals.
Figure 3: Stakeholder engagement and consultation methods
Screening Outcomes and Follow-Up
Participants will be treated according to the scan outcome as follows:
- No significant findings: Recommended to return for screening every two years.
- Low malignancy risk: Recommended to return in 12 months.
- Participants with moderate malignancy risk: Recommended to return in three months.
- High-risk findings or suspicion of lung cancer: Rapid referral to a specialist linked to a multidisciplinary team for clinical assessment and follow-up.
Program Launch
The LCSP will commence screening by July 2025.
Additional Resources
For more information, visit the Cancer Australia website: Cancer Australia Lung Cancer Screening.
Source for figures 1 and 2 can be found here
