Facing a diagnosis can be a daunting journey, rife with uncertainty and difficult decisions. Among these decisions is the choice of whether to participate in a clinical trial. While the prospect may initially seem overwhelming, it’s essential to recognise the potential benefits and weigh them against the uncertainties.
In this guide, we’ll explore five critical factors to consider when contemplating clinical trial participation, empowering patients to navigate this complex terrain with confidence and clarity.
The unknowns of clinical trials
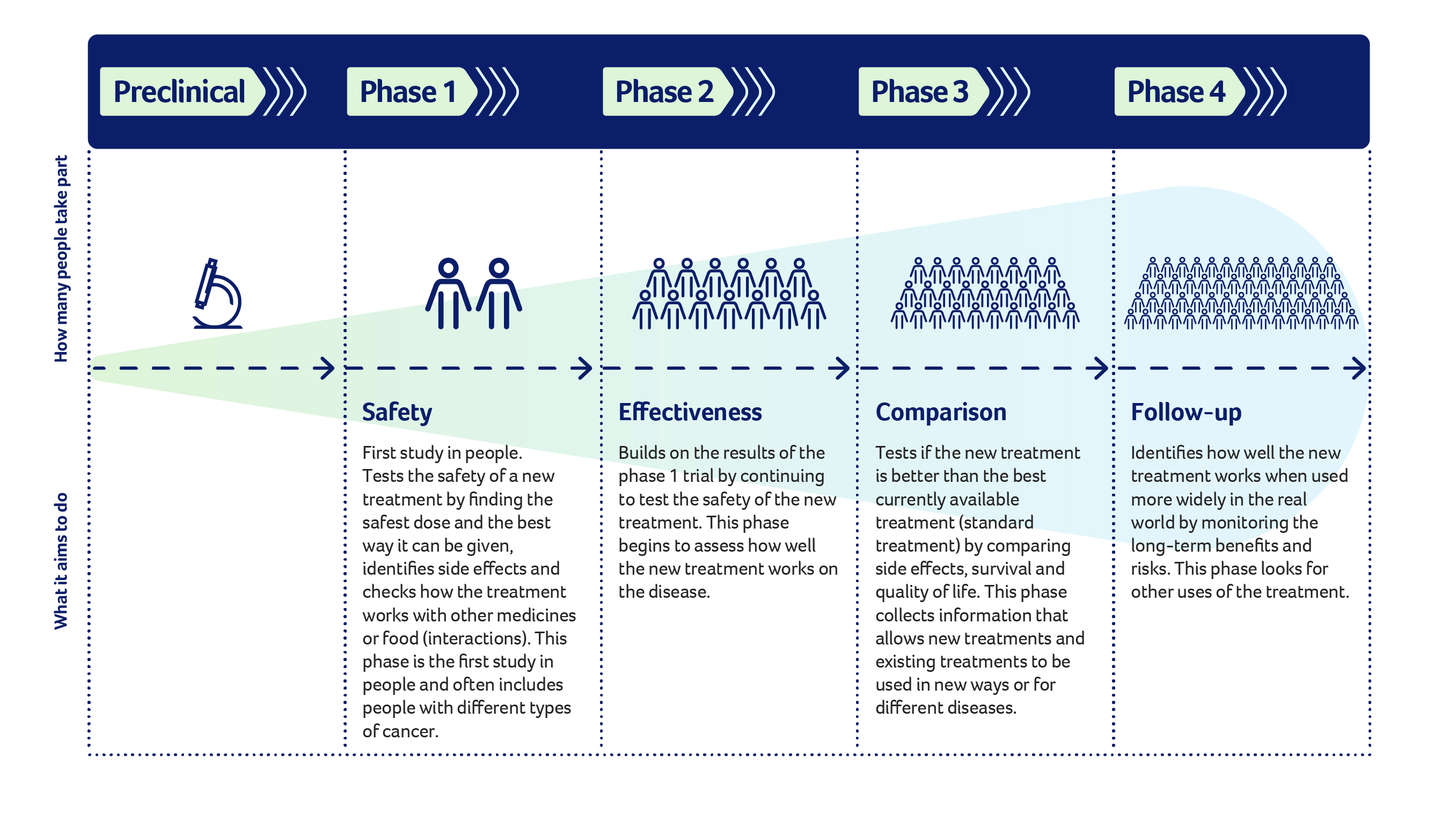
Clinical trials are ventures into uncharted territory, where new treatments are put to the test. Regardless of the trial’s phase, uncertainties abound.
From unknown side effects to the efficacy of the treatment in diverse patient populations, there’s much to ponder.
However, knowledge is power. Ensure you have read the consent form and engage with your clinician to unravel these uncertainties. Ask probing questions to obtain as much information as possible. Understanding the risks and potential benefits is key to making an informed decision.
Different healthcare teams
Entering a clinical trial may introduce you to a new ensemble of healthcare professionals or reframe your interactions with existing ones. From clinical trial nurses to coordinators and investigators, you’ll encounter a diverse array of experts dedicated to advancing cancer treatment. While the faces may change, the overarching goal remains constant: to find the best possible treatments for patients.
Embrace this collaborative effort, recognising that each member of the team plays a vital role in your journey. Getting to know your new team and respecting their efforts will put you at ease in this process.
Risks associated with clinical trials
Every clinical trial comes with its own set of risks, outlined meticulously in the Participant Information and Consent Form (PICF). Think of this document as your guidebook, offering insights into potential side effects and uncertain outcomes. Take the time to digest its contents thoroughly.
Adverse events, or unexpected side effects, play a pivotal role in the evaluation of medical interventions within clinical trials. During the clinical trial phase of drug development, fewer patients have been exposed to the drug so not all information about side effects is known. Pharmaceutical companies meticulously compile data on the effects of their drugs across various trials, documenting both anticipated and unforeseen reactions in an investigator brochure. This document must accompany a clinical trial and it is updated annually and distributed to all investigators working on the clinical trial.
In addition, all adverse events, regardless of severity or presumed cause, are diligently recorded during clinical trials. It is a collaborative effort between clinicians and pharmaceutical professionals to discern whether these events are directly linked to the drug being tested or are incidental occurrences.
A side effect that is believed to be related to the drug and not yet known will be rapidly reported and evaluated. Listings of these side effects are distributed to the clinical team on any clinical trial using the same drug, and are regularly reviewed to ensure that your trial is safe to continue. This process is conducted under stringent regulatory guidelines, ensuring appropriate safety oversight in the evaluation of new treatments. By meticulously documenting and analysing adverse events, researchers can enhance patient safety and refine our understanding of a drug’s potential benefits and risks.
Discuss any concerns with your healthcare team, leveraging their expertise to navigate the complexities of risk assessment. It is okay to seek information from another healthcare professional to gather additional information and insight. Ultimately, the decision to participate hinges on a careful balancing of risks and potential benefits.
Time and protocol
Participating in a clinical trial often entails adherence to a predefined protocol governing treatment procedures, appointments, and data collection processes. This protocol may necessitate adjustments to your daily routine or medication regimen. You may need to stop certain medication and be required to have study visits that are longer than normal visits. If required, this information will be in the consent form.
Before committing, take stock of these requirements. Consult with your healthcare and support team to assess the feasibility of accommodating these changes in your life. Open communication is key to ensuring that the trial aligns with your lifestyle and health goals.
Acceptance of uncertainty
Signing the consent form marks the beginning of your journey into the clinical trial realm. However, it’s crucial to acknowledge the possibility of non-selection. Initial screening tests may reveal that the trial is not a suitable fit for you, primarily due to safety considerations. While this may be disheartening, rest assured that your clinician will continue to provide you with the best possible care, prioritising your well-being above all else. Lean on your support system during this time, drawing strength from their unwavering encouragement and understanding.
Participating in a clinical trial is a deeply personal decision, shaped by a myriad of factors. By carefully considering the unknowns, embracing collaboration with healthcare teams, understanding risks, evaluating time commitments, and accepting uncertainties, you can approach this decision-making process with clarity and confidence. Ultimately, the choice to participate in a clinical trial is a testament to your resilience and commitment to advancing medical science for the betterment of all.
Where do I find clinical trials?
If you are interested in participating in clinical trials there are various resources to find trials that align with your medical condition and treatment preferences. The Australian Clinical Trials has the most comprehensive databases for finding clinical trials.
Additionally, TOGA supports clinical trials for non-small cell lung cancer (NSCLC), small cell lung cancer (SCLC), mesothelioma, other thymic malignancies, supportive & palliative care, and translational research.
